What an OCS Physical Therapist Actually Does
Orthopedics is broad, so an OCS clinician becomes the hub for many conditions: post-op rehab (shoulder, hip, knee, spine), sports injuries (tendinopathy, muscle strains), and persistent aches that didn’t budge with generic exercise sheets. Beyond picking exercises, they refine loading dosage (how much, how often, when to progress), spot red flags that need imaging or referral, and coach you on the long game—sleep, stress, and return-to-sport timelines.
A hallmark of OCS care is individualization. Two runners with the same “IT band pain” might get very different plans based on strength asymmetries, stride mechanics, tissue irritability, and training errors. That tailoring is where specialists often save weeks (or months) of trial and error.
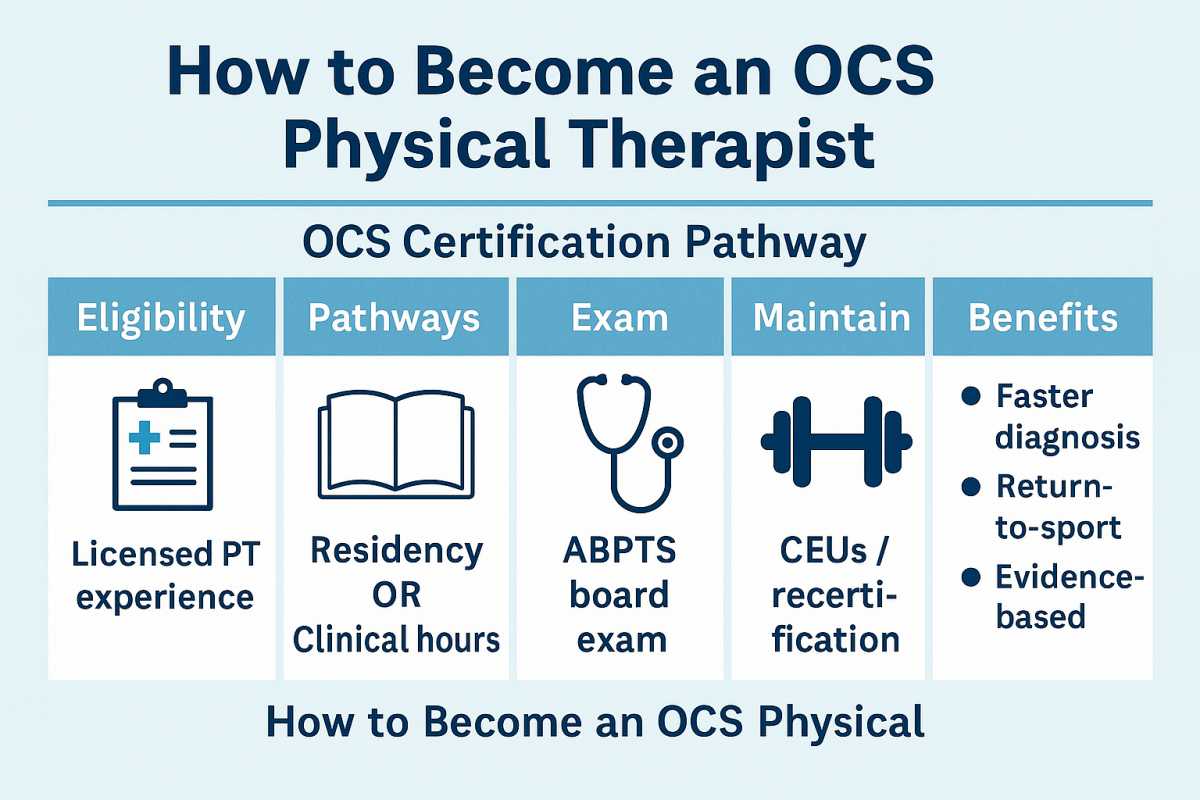
How a PT Becomes OCS Certified
To sit for the orthopedic board exam, a PT first completes a professional DPT (or equivalent), holds an active license, and then builds advanced orthopedic experience. There are two common pathways:
-
Accredited residency in orthopedics (intense, mentor-heavy year), or
-
Clinical hours route—typically a few thousand hours in orthopedic practice over several years.
After meeting eligibility, candidates take a comprehensive specialty exam covering everything from biomechanics to post-op protocols and complex case reasoning. Certification isn’t “set it and forget it” either; an OCS Certified Physical Therapist maintains the credential with ongoing professional development and periodic recertification focused on continuing competence.
Want the official criteria in one place? Check the ABPTS Orthopaedic Clinical Specialist overview (one link is enough for this article).
Why Patients Seek an OCS (Benefits you can feel)
Faster clarity. Specialists shorten the “what’s actually wrong?” phase. If you’ve bounced between providers or Google rabbit holes, that clarity alone is a relief.
Smarter progressions. Anyone can hand you exercises; OCS clinicians dial in volume, intensity, and tempo so tissues adapt without flaring.
Integrated manual + loading. Hands-on work can help—when paired with the right strengthening and movement retraining. OCS providers tend to blend both, instead of relying on passive care.
Return-to-sport criteria. Objective strength tests, hop series, and symmetry metrics help decide when it’s safe to cut, pivot, or sprint again—not just “it feels okay.”
Related Article: Pediatric Orthopedic Expert Witness
Conditions That Commonly Land in OCS Care
-
Post-surgical rehab (meniscus, rotator cuff, labrum, ACL, total joints)
-
Tendinopathies (Achilles, patellar, gluteal, lateral elbow)
-
Spine pain (disc-related, facet, movement coordination deficits)
-
Stress reactions & bone-load issues in runners
-
Shoulder impingement/instability and hip impingement (FAI)
-
Adolescent sports injuries (growth-plate aware loading)
Do You Need an OCS for Good Care?
Not always. Plenty of excellent generalist PTs get great outcomes. But if you’ve got a complex surgical rehab, a recurring sports injury, or a case that hasn’t improved with standard plans, an OCS can be worth seeking out—especially when you need nuanced progressions or sport-specific testing before you return to full throttle.
What a First Visit Feels Like (with an OCS)
Expect a deep dive into your training history, sleep, stress, prior flares, and goals. Assessment typically includes movement screens (squat, lunge, single-leg stance), joint mobility, strength/endurance tests, and task-specific drills (e.g., runner step-down, overhead reach for throwers). You’ll leave with a precise plan: 2–4 priority exercises (with reps/tempo), a weekly progression map, and avoid/do lists to calm symptoms while building capacity.
How to Choose the Right OCS for You
-
Sport or activity match. If you’re a runner, find someone who treats runners weekly; if you lift, pick a clinician who understands programming.
-
Measures that matter. Do they test strength (hand-held dynamometer, isokinetics), range, and function—or just eyeball?
-
Communication. You should understand why each exercise is in your plan, when to progress, and what pain levels are acceptable.
-
Access. One-on-one time beats crowded gyms. Ask how many patients your therapist treats per hour.
Related Article: Choosing an Ortho Bionomy Practitioner
Quick FAQ
Is OCS a separate license?
No, it’s a board certification beyond your PT license—evidence of specialty depth, not a new license.
How long is the credential valid?
Specialists maintain certification through continuing competence and periodic recertification. It’s designed to keep skills current rather than be a one-and-done exam.
Will insurance care if my PT is OCS?
Most plans don’t pay differently for OCS, but the quality and efficiency of care can still save you time and follow-up visits.
Bottom Line
If you’re dealing with a stubborn orthopedic problem—or prepping for a big comeback after surgery—an OCS Physical Therapist can be a smart move. The extra training shows up where it counts: clearer diagnoses, tighter loading progressions, and safer return-to-sport decisions. And when you see “OCS Certified Physical Therapist” next to a name, you can reasonably expect someone who’s invested in going beyond the basics—so you can get back to moving the way you actually want to move.
